Back of Heel Surgeries: Your Complete Guide
Exhaust Conservative Treatment for Back of Heel Pain First
If you have exhausted all the possible conservative treatments for the pain at the back of your heel, and you’re still having pain then it’s time to talk about surgery.
All surgery comes with risks, and this is why we recommend avoiding surgery until it’s absolutely necessary.
Make an appointment to see us in our Seattle clinic or via telehealth to discuss your specific situation.
Back of Heel Surgery Considerations
In order to reach the back of your heel to perform surgery, you will need to be lying on your stomach for the surgery. This is more difficult for individuals who may have breathing problems, like sleep apnea, snoring and for overweight individuals but the anesthesiologist is skilled in handling these situations.
Be sure to see our Pre Surgery Preparations page and thoroughly read about everything you should know about foot surgery before you have it.
Types of Back of Heel Surgery:
The procedure for each heel surgery is different depending on what your specific heel condition is. See below for details on:
- Haglund’s deformity (a.k.a.: retrocalcaneal exostosis, Mulholland deformity, and ‘pump bump) surgery
- Bone spur (aka Achilles tendon insertional calcification) surgery
- Achilles tendon bursa surgery
- Achilles tendon debridement (aka Achilles tendon debulking)
The Haglund’s Deformity Surgery:
(a.k.a.: retrocalcaneal exostosis, Mulholland deformity, and ‘pump bump)
The haglund’s deformity surgery will start like any heel surgery, as described above. Once the anesthesiologist has safely started your anesthesia we begin the operation.
During the surgery:
- The skin is opened with a specially designed incision to minimize scarring. We generally use a curve shaped incision because it heals better than a straight midline incision.
- The Achilles tendon will be partially detached from the calcaneus. This is necessary to view and remove the bony bump that makes a haglund deformity.
- The bony bump on the calcaneus will be carefully shaved off. Knowing how much to remove is an important skill that an experienced surgeon will know best.
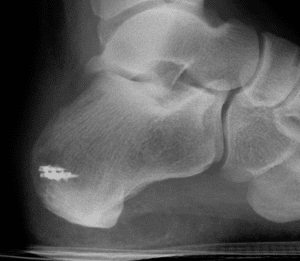
- The Achilles tendon will be reattached to the newly shaped calcaneus with several small anchors. Some of these anchors are made out of metal with strong thread attached. If you are allergic to certain metals, it’s important to discuss that with your surgeon before the operation.
- The skin is closed with stitches and a bandage is placed over the surgical site.
- You will have a splint placed on your foot that will minimize the movement at your ankle joint.
Achilles Bone Spur Surgery:
(Achilles Insertional Calcific Tendonosis)
The Achilles bone spur surgery will start like any heel surgery, as described above. The Achilles bone spur surgery is very similar to the haglund’s deformity surgery.
During the surgery:
- First the skin over the Achilles tendon and part of the calcaneus is opened with a skillfully designed incision.
- The surgeon will delicately dissect down through the tissue to the Achilles tendon and expose it.
- The Achilles tendon is opened and partially detached from the calcaneus to gain access to the spur. The tendon is then dissected off the bone spur.
- With the Achilles tendon temporarily detached, your doctor can shape the calcaneal bone so that the painful protrusion causing your symptoms is no longer present.
- Occasionally, you may have a painful fluid filled sack around the insertion of your Achilles tendon called a bursa. This bursa can be removed during surgery as it offers no benefit and may contribute to the pain you feel.
- Removing a bursa will likely not affect your healing, and your recovery from the procedure will be unchanged.
- The Achilles tendon may have been irritated for some time, causing it to thicken with scar tissue. If this is the case, the dead or diseased scar tissue around the Achilles tendon will be removed during your surgery before the tendon is reattached.
- Exactly as described in the haglund’s surgery, the Achilles tendon will be reattached, and the skin will be meticulously closed using stitches.
Recovery, risks and follow up for this procedure are identical to the haglund’s deformity surgery.
Retrocalcaneal Bursa Surgery:
The fluid filled bursa behind the Achilles tendon is also known as the retrocalcaneal bursa and it can be inflamed causing pain. Be sure to read about signs and symptoms of an inflamed bursa on our informative Back of Heel Pain page.
This is almost always treatable conservatively, and very rarely requires surgery on it’s own.
An inflamed painful bursa is often secondary to a bone protrusion such as the haglund’s deformity, or a bone spur. The bursa may be removed in a haglund’s surgery or in a bone spur removal surgery as an additional procedure.
If the bursa is removed surgically you will most likely not notice any difference in the appearance or function of your foot. The main difference will be the reduction in pain that accompanies removal of a bursa.
If a bursa surgery is added to any other back of heel surgery the recovery will be similar to the surgery it was added to, and no additional special treatments are necessary. The bursa removal will be performed through the same incision as the other surgery, and no additional incisions will be necessary.
Achilles Tendon Debridement:
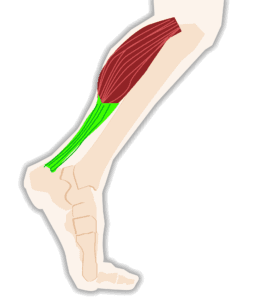
Your body adapts over time to protect itself, and when it comes to the Achilles tendon this can mean scar tissue formation when the tendon is
damaged. This damage can be acute, meaning the tendon is still inflamed and requires conservative treatment. Over longer periods of time chronic damage to the Achilles tendon will cause the body to build up thick scar tissue in and around the Achilles tendon.
Having a thick Achilles tendon doesn’t necessarily mean it’s stronger, and actually tends to weaken the tendon making it more likely to rupture.
If this is the case, the scar tissue can be removed surgically to repair the tendon.
Removing scar tissue from the Achilles tendon is called debulking, because it removes the bulky diseased tissue from the tendon. You may also hear this referred to as debridement.
This procedure can be performed on it’s own or with any combination of other back of heel procedures depending on the exact cause of your pain.
During the Achilles Tendon Debridement Surgery:
- Depending on the extent of the damage to the Achilles tendon, the skin incision may extend from the back of heel to several centimeters up the back of your calf.
- Your surgeon will dissect down to the Achilles tendon and inspect it to determine how much debulking is necessary.
- The next steps depend heavily on what your unique Achilles tendon looks like. The tendon will likely need to be opened and the diseased tissue will be removed from the inside. The extent of the incision and the debridement is guided by your tendon, and what the experienced surgeon sees during surgery.
- Once the dead tissue is removed the tendon will be repaired. This can involve sewing the tendon back together, and possibly including a tissue graft or stem cell placement around the surgical area. If this is the case, your surgeon will discuss it with you far in advance of the surgery.
- Once the tendon is repaired, the skin will be closed and you will be placed in surgical bandages and a splint to prevent movement of the ankle joint.
The Achilles tendon debridement surgery recovery time and procedure should be exactly the same as with any other back of heel surgery.
There is an increased likelihood that you will need physical therapy after your surgery to teach you how to stretch the Achilles and safely return to physical activity.
One complication that is more common with the Achilles tendon debridement is the possibility for the tendon to rupture if you return to activity too fast or attempt an activity that is too strenuous for the recovering tendon. You can avoid this complication by following your surgeon’s recovery plan closely, and avoiding weight bearing until you are fully recovered.
Recovery from Most Back of Heel Surgeries:
After your surgery you will wake up with the splint on your leg and you will be transported to the recovery room. You may feel a little groggy after surgery, which is normal and should wear off in several hours.
You will likely not feel any pain after the surgery for at least 6-10 hours because of the injectable local anesthetic used during the surgery. If you do feel pain it is important to notify your surgeon and there are many different ways that your pain can be reduced.
For the first few days after surgery you should plan to stay at home, relax and spend the majority of your time seated with your leg elevated on 1-2 pillows. You will want to have an ice pack available to help with any pain and swelling you experience.
You may want to have a special pillow, or multiple pillows that can support your leg while not placing any pressure on the surgical site.
You will not put any weight on your foot, or move your ankle for 4-6 weeks after surgery. The exact point at which you can start transitioning to putting weight on your foot depends on how you are healing, and your surgeon will guide this decision during the follow up visits after surgery.
You will need a knee scooter or crutches after surgery to help you avoid putting weight on the foot. You will wear a splint until your first follow up visit with your surgeon, then you will be transitioned to a surgical boot. You will wear the surgical boot until you are fully weight bearing on the foot, and you do not need the crutches anymore.
Risks of Back of Heel Surgery:
Certain risks come with any surgery, including the risk of pain, infection, nerve injury, blood vessel injury, deep vein thrombosis (DVT), pulmonary embolism (PE), bleeding, the surgical site not healing, and the need for another surgery. The chances of these complications occurring are very low, and can be lowered even more by you following your surgeon’s instructions diligently. For more information on these complications be sure to see our Pre-Surgical Planning page.
Specifically for back of heel surgery one of the most common complications is wound healing difficulty. Some people lay their foot on a pillow and put excess pressure on the incision. This can cause the surgical site to not heal properly and possibly break open. If this happens the Achilles tendon underneath the incision is at risk for infection, which can be serious. You can reduce your risk of developing this complication by reducing the pressure on the back of your heel while you are recovering from surgery.
With back of heel surgery it is always important to follow your doctors guidelines over walking and weight bearing. There is a significant risk that early walking or weight bearing could damage the surgical site, or pull the bone anchors out of the calcaneus.This would require a second surgery, which we would like to avoid.
Rarely, the body can have a reaction to your surgery which results in calcium deposits around the surgical site. The reason for these little calcium deposits is clear in medical literature, but it is a known complication to back of heel surgery. If your body develops this calcium deposit reaction, you may require another surgery to remove the small hard calcium stores.
When will I be able to walk again after back of heel surgery?
While every person is different, most people are able to walk by 8-9 weeks after surgery. Some additional physical therapy may be necessary. Usually you can walk in a boot 6 weeks after surgery.
Re-attaching the Achilles tendon to the heel bone is necessary for the haglund’s surgery and for Achilles tendon bone spur surgery, but can take a while to heal. You may need 5 to 12 months after your surgery to fully return to normal.
What kind of anesthesia is used?
Most back of heel surgery requires you to be placed on your stomach for the operation, because of this position you will most likely need general anesthesia. In some rare circumstances a type of anesthesia called a “regional block” can be used, if this is the case with your surgery we’ll discuss it with you well in advance.
Will I need physical therapy after my haglund’s surgery?
Yes, you may need to see a physical therapist after your heel surgery to help you get back to normal walking and activity. At the Foot and Ankle Center of Washington we fully value the role physical therapy plays in your recovery, and if we determine that you will benefit from it, we will be sure to refer you.
How often will I see my surgeon after surgery?
You may see your surgeon 3-5 days after your surgery for the first check up. After this first visit, you will see your surgeon every few weeks to monitor your healing until you are walking normally again. Remember to call if you have any issues after surgery.
When will I be able to wear normal shoes again?
You can usually start wearing shoes 8-9 weeks after surgery and the transition will likely be gradual. A shoe with a heel may take pressure off the surgical site.
I need a back of heel surgery, what do I do next?
If you’ve been told that you need surgery, and you’d like a second opinion, please make an appointment with us at the Foot and Ankle Center of Washington and we’ll evaluate whether or not you are a good surgical candidate. We specialize in second opinions at the Foot and Ankle Center of Washington and we have an excellent reputation for avoiding surgery unless it’s the only remaining option.
When you’ve met with your doctor and tried every other possible conservative treatment first, you’re ready to talk about surgery.
Here at the Foot and Ankle Center of Washington in Seattle we have over 25 years of experience caring for back of heel pain both conservatively and surgically.
Make an appointment with us to determine what procedures are necessary, and we’ll build a custom surgery plan for you complete from preparation to recovery.
References:
- Tu P. Heel Pain: Diagnosis and Management. Am Fam Physician. 2018;97(2):86‐93.
- Traina F, Perna F, Ruffilli A, et al. Surgical treatment of insertional Achilles tendinopathy: a systematic review. J Biol Regul Homeost Agents. 2016;30(4 Suppl 1):131‐138.
- Wiegerinck JI, Kok AC, van Dijk CN. Surgical treatment of chronic retrocalcaneal bursitis. Arthroscopy. 2012;28(2):283‐293. doi:10.1016/j.arthro.2011.09.019